How Dentists Treat Gingivitis?


Understanding Gum Disease
Gum disease is a significant dental concern that can affect individuals of all ages. It begins with gingivitis, a condition marked by inflammation of the gums, commonly caused by the accumulation of bacterial plaque in the mouth. As this plaque builds up, it can lead to serious health issues if left untreated.
The Impact of Plaque Build-Up
Plaque is a sticky biofilm that forms on teeth as a result of food particles and bacteria. It can harden into tartar if not removed through regular brushing and flossing. According to the Cleveland Clinic, dentists treat plaque using special instruments during dental checkups. They also recommend maintaining good oral hygiene practices, such as brushing and flossing daily, to prevent buildup.
Age Group Percentage of Adults with Gum Disease
30 and older 47%
65 and older 70%
This table highlights the prevalence of gum disease among adults, indicating that almost half of all adults over 30 experience some form of gum disease [1].
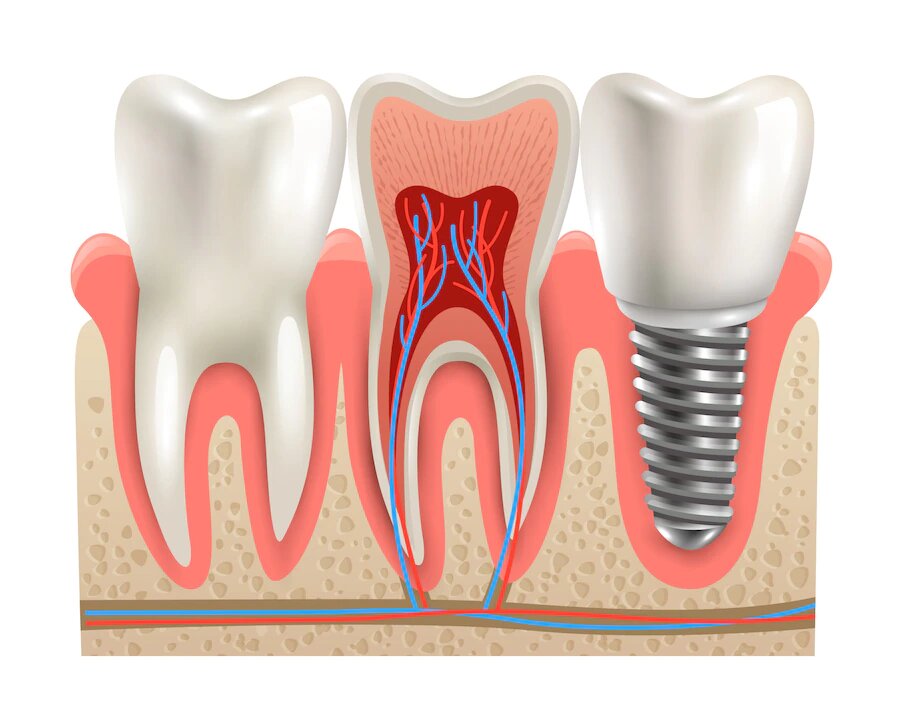
Progression from Gingivitis to Periodontitis
If gingivitis is not treated adequately, it can progress to periodontitis, a more severe form of gum disease. This stage involves inflammation that not only affects the gums but can also lead to bone loss in the jaw. Immediate treatment is essential, as gingivitis is curable when addressed early. Individuals experiencing symptoms such as swollen or bleeding gums should schedule an appointment with their dentist [1]. Regular dental checkups are crucial, as early detection can help prevent the progression from gingivitis to periodontitis.
By understanding the impact of plaque buildup and the possible progression of gum disease, individuals can take proactive steps in their dental care, ensuring healthier gums and reducing the risk of severe complications. For further information on maintaining gum health, please refer to our article on why you should see a dentist every six months.

Diagnostic Procedures for Gingivitis
Correctly diagnosing gingivitis is crucial for effective treatment and recovery. Dentists utilize specific diagnostic procedures to assess the extent of gum disease and take appropriate action. This section will discuss two primary procedures: medical and dental history review, and clinical examination for plaque and inflammation.
Medical and Dental History Review
The diagnosis process begins with a thorough review of the patient's medical and dental history. Dentists ask about any previous dental issues, current symptoms, and habits that may contribute to gum disease. They inquire about the following:
Medical History
- Do you have any chronic illnesses (e.g., diabetes) or take regular medications?
Dental History
- Have you experienced any previous issues with your gums or teeth?
- When was your last dental visit?
Oral Hygiene Habits
- How often do you brush and floss your teeth?
- Do you use mouthwash regularly?
This comprehensive history helps dentists identify risk factors and underlying conditions that may contribute to the development of gingivitis. Additionally, understanding the patient's history can guide decisions for necessary treatment.
Clinical Examination for Plaque and Inflammation
Following the initial history review, the dentist will conduct a clinical examination. This involves closely examining the teeth, gums, mouth, and tongue for signs of plaque build-up and inflammation. Key aspects of this examination include:
Pocket Depth (mm) Gum Health
1-3 Healthy
4-5 Early Gum Disease (Gingivitis)
6+ Advanced Gum Disease (Periodontitis)
In some cases, the dentist may also recommend dental x-rays to check for bone loss surrounding the teeth, which may indicate a progression of the disease [2].
By combining a review of medical history with a clinical examination, dentists can accurately diagnose gingivitis and initiate the necessary treatment plan to restore gum health. Regular dental cleanings and check-ups greatly enhance the diagnosis of oral health issues like gingivitis as well [3].

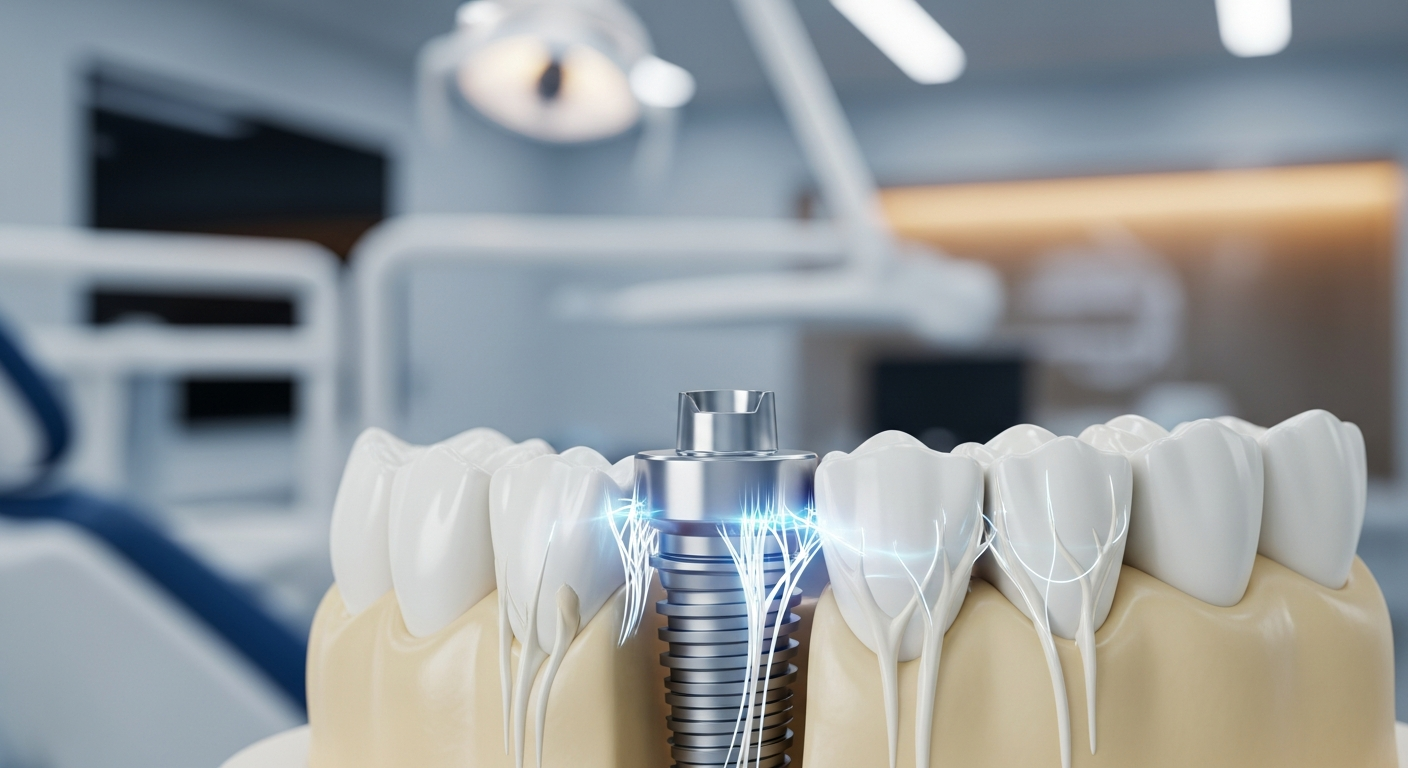
Treatment Options for Gingivitis
Addressing gingivitis effectively hinges on the treatment strategies employed. There are both non-surgical and surgical avenues to explore depending on the severity of the gum disease.
Non-Surgical Approaches
Non-surgical treatment is often the first line of defense against gingivitis and can be quite effective. This method mainly includes:
Treatment Method Description
Professional Dental Cleaning Removal of plaque and tartar from teeth and gums
Scaling and Root Planning Deep cleaning for gum reattachment
Antibiotics Medication to combat bacteria
Prompt treatment of gingivitis usually reverses symptoms and prevents progression to more severe gum issues or tooth loss. Maintaining good oral hygiene at home and avoiding tobacco use further reinforces these treatment efforts [4].
Surgical Interventions for Severe Cases
In more advanced stages of gum disease, surgical intervention may be required. Options for severe gingivitis include:
Purpose Description
Flap Surgery Moves tartar and smooths damaged bone surfaces
Bone Grafts Replaces lost bone due to gum disease
Soft Tissue Grafts Restores gum tissue to protect tooth roots
Each treatment option is discussed with patients based on the severity of their condition [5]. Understanding how dentists treat gingivitis can empower individuals to take proactive steps toward oral health.
Essential Care for Gum Health
Maintaining optimal gum health is a vital part of preventing and treating gingivitis. Essential care involves regular dental visits and diligent home oral hygiene practices.
Role of Regular Dental Cleanings
Regular dental cleanings and check-ups are fundamental for sustaining good oral health. These appointments allow dentists to diagnose and treat issues like gingivitis effectively. The American Dental Association recommends visiting the dentist at least twice a year for cleanings and preventative care. During these visits, a professional cleaning removes plaque and tartar buildup that regular brushing alone may not address. As noted by Amazing Smiles PC, this helps in preventing gingivitis symptoms and stops the progression to more severe gum diseases.
Frequency of Dental Visits
Frequency Purpose
Every 6 Months Preventive care and early diagnosis
Every 3-4 Months Recommended for those with existing gum disease
Regular check-ups also allow dentists to monitor patients' gum health and ensure any symptoms of gingivitis receive prompt treatment. Quick action can reverse symptoms and prevent the development of periodontitis, as emphasized by the Mayo Clinic.
Maintaining Good Oral Hygiene at Home
Good oral hygiene is crucial for the effective management of gingivitis. This includes proper brushing, flossing, and using other dental care tools. Here are some key practices to adopt:
Successful gum care at home significantly impacts overall gum health and potential treatment outcomes for conditions like gingivitis. Adhering to these practices alongside regular dental visits will improve oral health and prevent future complications. If any symptoms of gingivitis arise, a quick visit to the dentist is essential to seek proper treatment as recommended by the Mayo Clinic.
Preventive Measures for Gingivitis
Taking proactive steps can significantly reduce the risk of developing gingivitis. Effective brushing techniques and proper dental care routines are essential for maintaining healthy gums.
Effective Brushing Techniques
Brushing teeth correctly plays a crucial role in preventing gum disease. Individuals should aim to brush at least twice a day using the right toothbrush. Here are some key tips for effective brushing:
To maintain optimal gum health, following a routine that includes proper brushing techniques is crucial. For additional advice on maintaining an overall effective oral care regime, visit our article on why you should see a dentist every six months.
Importance of Flossing and Dental Checkups
In addition to effective brushing, flossing daily is essential for cleaning the spaces between teeth where plaque accumulates. Flossing helps remove food particles and reduces the risk of gum inflammation. The following table summarizes the recommended dental care routine:
- Brush Teeth: Twice a day
- Floss: At least once a day
- Dental Checkups: Every six months
Regular dental visits are vital for preventing gingivitis. During these appointments, dentists can remove plaque build-up and polish teeth, providing protection against bacteria James Lake, DDS. Following your dentist's recommendations and maintaining a consistent oral hygiene routine will help in returning healthy gum tissue within days to weeks [6].
By implementing effective brushing techniques and making flossing a daily habit, individuals can significantly lower the risk of gingivitis and ensure their gums remain healthy. Regular checkups are equally important for early detection and intervention.
Dietary Tips for Oral Health
Maintaining a balanced diet is crucial for optimal dental health. The foods individuals consume can significantly impact their oral hygiene, affecting their risk for conditions such as gingivitis and dental caries.
Impact of Diet on Dental Health
Diet plays a key role in the development of dental issues. Excessive sugar consumption positively correlates with the development of dental caries. Every time sugar is consumed, enamel demineralization occurs, and the frequency of sugar intake exacerbates this problem [7]. Foods that adhere to dental surfaces can increase the risk of tooth decay. Even non-sticky foods, like sugary beverages, significantly elevate this risk.
Effective dietary habits include:
Limit Sugar Intake
Aim for less than 15 to 20 kg per person per year.
Frequency of Sugar
Consume sugary foods and drinks no more than four times daily.
Stimulate Saliva Production
Eat foods like hard cheeses and peanuts.
These strategies can help protect enamel and maintain oral health.
Foods to Promote Healthy Gums
- Leafy greens rich in vitamin C and calcium
- Crunchy fruits and vegetables like apples and carrots
- High-fiber foods that stimulate saliva production
- Foods rich in omega-3 fatty acids like salmon and mackerel
- Dairy products high in calcium and probiotics
- Green tea for its anti-inflammatory properties
- Raw onions for their antibacterial qualities
- Nuts and seeds high in vitamin E and minerals
- Citrus fruits rich in vitamin C
- Whole grains for their B vitamins and iron content
- Plain yogurt with live cultures
- Celery sticks for natural teeth cleaning
- Firm fruits like pears for gum stimulation
- Sugar-free gum with xylitol
- Foods rich in CoQ10 like organ meats
By prioritizing these dietary choices, individuals can better protect their gums and teeth. For further information on dental health maintenance, explore the section on why you should see a dentist every six months.
References
- https://www.nidcr.nih.gov/health-info/gum-disease/more-info
- https://www.ada.org/resources/research/science-and-research-institute/oral-health-topics/periodontal-disease
- https://www.mayoclinic.org/diseases-conditions/gingivitis/symptoms-causes/syc-20354453
- https://www.perio.org/for-patients/gum-disease-information/
- https://www.mouthhealthy.org/all-topics-a-z/gingivitis
- https://www.who.int/news-room/fact-sheets/detail/oral-health















































.avif)










.jpg)


















.avif)


















.jpg)


